Abstract Objective: We present an unusual clinical presentation of a carotid artery pseudoaneurysm on a post-laryngectomy patient with a history of carotid artery blowout and subsequent ligation of the carotid artery. Methods: Case report and literature review. Results: The patient presented with subtle cutaneous bleeding in the peristomal region as a sentinel exam finding for carotid artery pseudoaneurysm. Subsequent workup revealed a 3 cm carotid artery pseudoaneurysm of the proximal ligated vessel stump. The underlying mass effect of the pseudoaneurysm had caused cutaneous vessel dilation and subsequent bleeding. The patient underwent successful endovascular stenting to bypass the aneurysm without complication.
Conclusion: This case describes a novel and unusual clinical presentation of a carotid artery pseudoaneurysm and demonstrates the importance of subtle physical exam findings, clinical history and a comprehensive knowledge of pathophysiology. Keywords: Carotid artery, pseudoaneurysm, aneurysm.
Introduction A pseudoaneurysm, or false aneurysm, involves a rupture of all three layers of an arterial wall into an adjacent tissue cavity with persistent communication between the artery and that cavity. This differs from a true aneurysm in which the artery walls remain intact though expanded. Pseudoaneurysms are commonly encountered after the tunica media has been thinned and/or compromised, such as in trauma, surgery, arteriosclerosis, and infection.
† Fully covered, partially covered and uncovered stents in multiple sizes are available. Problem of tumour ingrowth and reduce the rate of stent occlusion. Covered stents significantly reduced the need for. Mac 16 Created Date.
In this case we discuss carotid artery pseudoaneurysm, a rare but potentially lethal clinical entity, with a uniquely complex clinical presentation. Case Report A 62 year old female with a history of T3N0M0 glottic squamous cell carcinoma 17 years prior (treated with chemoradiotherapy) developed a recurrence with extension into the supraglottis. Recommendation was for laryngectomy.
However, the patient pursued a second opinion at an outside institution and subsequently opted for re-irradiation and additional chemotherapy. Unfortunately, the patient developed significant laryngeal dysfunction and aspiration secondary to chondroradionecrosis, which required total laryngectomy approximately 1 year later. Post-laryngectomy, the patient’s post-operative course was complicated by pharyngocutaneous fistula and subsequent right carotid artery blowout in December 2011. Amazingly, the patient’s life was saved with emergent ligation and the fistula was covered with a pectoralis major myocutaneous flap. 5 months later, the patient returned to clinic with complaint of granulation tissue, erythema and minor bleeding around the laryngectomy stoma. Biopsy of peristomal tissue was performed with no evidence of malignancy, and the patient was not taking any anticoagulant medications. The peristomal bleeding tissue was treated with silver nitrate and the patient was placed on a 14-day course of clindamycin with minor improvement in erythema but persistent minor bleeding. Several nights later the patient presented to the emergency department complaining of additional minor bleeding around the stoma as well as shortness of breath. Though she was afebrile and labs were within normal limits (WBC: 6.6; Hct: 37, INR: 1.1/PT 12.6 / PTT 25), the patient was admitted for observation.
Blood cultures were negative. Given the patient’s history of iodine allergy and history of bleeding from the neck, an MRI/MRA was performed. A 3 centimeter pseudoaneurysm was noted to originate from the right proximal carotid artery remnant at the brachiocephalic artery FIGURE 1. Figure 1: T1-Weighted Magnetic Resonance Image with Gadolinium; Right Common Carotid Artery Pseudoaneurysm (White Arrow) Noted on (A) Coronal, (B) Axial, and (C) Sagittal Views Cardiothoracic surgery was consulted. Steroid pretreatment was undertaken for the patient’s iodine allergy prior to angiography, which further confirmed the pseudoaneurysm and endovascular repair was undertaken.
Right common femoral artery was accessed with an 18-gauge angiographic introducer needle. Wire was advanced to the aortic arch and utilizing a VTK catheter brachiocephalic artery was cannulated.
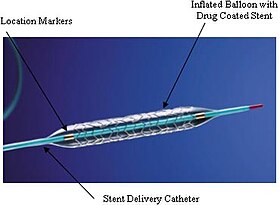
A selective angiogram of the brachiocephalic artery was performed which demonstrated a large pseudoaneurysm originating at the base of the right carotid artery with patent inferior mammary artery and vertebral arteries. Then a stiff-angled Glidewire was advanced out to the brachial artery in the arm and a long 7-French 90 cm Terumo destination sheath was advanced into the origin of the brachiocephalic artery. Another selective angiography was performed again to delineate the anatomy and a 9 mm x 38 mm Atrium iCAST covered balloon mounted stent was advanced into the level of the brachiocephalic artery just proximal to the vertical artery and the inferior mammary artery covering the lesion. The stent was deployed without difficulty.
Completion angiography demonstrated exclusion of the pseudoaneurysm with brisk flow out to the arm and retained patency of the IMA and vertebral arteries FIGURE 2. Figure 2: Magnetic Resonance Angiogram; (A) Pseudoaneurysm (White Arrow) Noted at Proximal Stump of Previously Ligated Right Common Carotid Artery as it Branches off the Brachiocephalic Artery. (B) Covered Endovascular Stent (Arrow) Successfully Deployed to Bypass Pseudoaneurysm The patient tolerated the procedure well without any complications. After successful stent deployment, the peristomal bleeding was noted to subside and patient was started on Aspirin 81mg daily.
Patient had uncomplicated hospital course and was discharged home after 8 days in the hospital. Postoperatively, the patient was closely followed in an outpatient setting.
Patient returned to the emergency room several months later with complaint of chest pain. CT angiogram of chest was performed to evaluate for possible pulmonary embolism which showed pulmonary nodules. CT guided biopsy confirmed pulmonary metastasis and patient is currently undergoing palliative chemotherapy. Discussion Common carotid artery pseudoaneurysms are uncommon, perhaps representing 14% of all common carotid aneurysms and as few as 1 in 800 aneurysms overall, as described by El-Sabrout et al (2000). While they are most commonly caused by either penetrating or blunt trauma, Lyons et al (1997) and Mathur et al (2010) list a wide range of more infrequent causes, including arteriosclerosis, dissection, vasculitis, infection (mycotic aneurysm), radiation, idiopathic, and surgery (such as patch angioplasty following endarterectomy). Although surgery is documented to be a common cause of pseudoaneurysm formation, common carotid artery ligation alone has not specifically been associated with the development of carotid or brachiocephalic artery pseudoaneurysms in the literature. When untreated, the majority of patients will develop stroke (50%) with early reports discussed by Hertzer (2000) and Zwolak (1984) indicating a mortality rate of 60-70%.
Patients with a common carotid artery pseudoaneurysm classically present with a neurologic deficit due to compression of a nerve or intracranial thromboembolism. In up to 90% of common carotid artery pseudoaneurysms, a unilateral pulsatile neck mass is present, typically immediately inferior to the angle of the jaw.
As discussed by Bergan and Hoehn (1965), this presentation may be similar to that of a coiled or kinked carotid artery, which can be differentiated on physical exam by the direction of pulsation (coiled arteries will pulsate parallel to the vessel, while the pulsation of a pseudoaneurysm radiates laterally). In this case, no pulsation was palpable given the patient’s previous vessel ligation relatively low in the neck and overlying pectoralis flap. Interestingly, as in this case, a pseudoaneurysm may present with signs and symptoms of venous stasis caused by compression and subsequent dilation of nearby veins. Ultrasound, CT, MRI, and/or angiography may be utilized to confirm the diagnosis and establish specific measurements of the aneurysm and its relationship to the surrounding anatomy.
Treatment typically requires surgical repair of the pseudoaneurysm. Depending on the aneurysm size and characteristics,vein grafting or primary end-to-end anastomosis may be performed. Direct ligation may be used in cases of uncontrollable hemorrhage. Fortunately, endovascular approaches which involve stent grafting are gaining favor as the preferred treatment strategy for common carotid artery pseudoaneurysms.
Additionally, Lee et al (2013) recently used percutaneous thrombin injection with a distal embolic protection device to successfully treat a common carotid artery pseudoaneurysm. Moller et al (2012) similarly performed emergent percutaneous thrombin injection at the bedside for CCA pseudoaneurysm, but without cerebral protection. The procedure was successful and resulted in no neurologic complications. Percutaneous thrombin injection, both with and without temporary balloon occlusion, has well-documented efficacy for the treatment of femoral artery pseudoaneurysms with highly infrequent embolic complications. Additional data regarding the safety and efficacy of intravascular approaches of the carotid arteries is warranted as these treatment strategies do have the risk of symptomatic thromboembolization from the pseudoaneurysm, as documented by Longo and Kibbe (2005). Conclusion Carotid artery pseudoaneurysm is a rare but potentially lethal clinical entity often manifesting silently with minimal clinical exam findings until uncontrolled rupture. This case presentation demonstrates a novel description of cutaneous manifestation of common carotid artery pseudoaneurysm and the importance of subtle physical exam findings, awareness of the patient’s clinical history and a comprehensive knowledge of pathophysiology.
References Bergan, J. “,” Annals of Surgery, 162:213-217.
– El-Sabrout, R. “,” Journal of Vascular Surgery, 3:701-712. – Hertzer, N. “,” Journal of Vascular Surgery,31:823-825. “,” Case Reports in Otolaryngology, 2012:5.
H., Tseng, I. K., Siegel, R. & Roychowdhury, S.
“,” Interventional Neuroradiology: Journal of Peritherapeutic Neuroradiology, Surgical Procedures and Related Neurosciences, 19. “,” Seminars in Vascular Surgery, 18(4)178-183. J., Barker, C. “,” Journal of Oral and Maxillofacial Surgery, 55:77—79.
N., Joshi, R. R., Nepal, A.
& Rauniyar, R. “,” Journal of Laryngology and Otology, 124(6)684-686. M., Logason, K., Karason, S.

Mri Safety Fda
& Thorisson, H. “,” Texas Heart Institute Journal, 39(5):696-8. W., Jang, J., Gustavson, S. “,” Circulation, 115:2666-2674. M., Whitehouse, W.
M., Knake, J. “,” Journal of Vascular Surgery, 1:415-422.